Scientists working to quell the COVID-19 pandemic have developed tests that detect antibodies in the blood of people who have previously been infected with the new coronavirus. These serology tests can provide important data on how COVID-19 is spreading through a population. There is also hope that the presence of certain antibodies may signify immunity to future infection—a possibility scientists are still investigating. Antibody tests do have potential shortcomings: they may detect ineffective antibodies, they do not indicate if an infection is still active, and they fail to detect infection if administered before antibodies develop. A new test's accuracy can also be difficult to determine because of a lack of data.
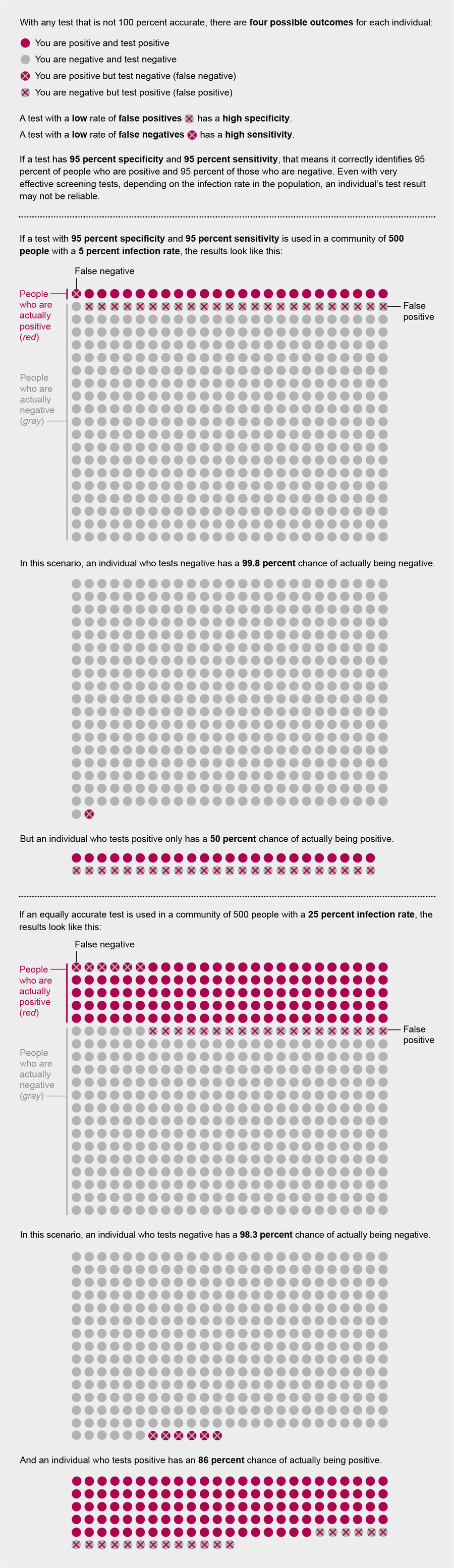
Still, such tests have been proposed as a way for individuals to find out if they have already been infected with the novel coronavirus. But a mathematical wrinkle makes these tests—and in fact, all screening tests—hard to interpret: even with a very accurate test, the fewer people in a population who have a condition, the more likely it is that an individual's positive result is wrong. If it is, people might think they have the antibodies (and thus may have immunity), when in fact they do not.
A positive screening test result for other diseases usually prompts follow-up testing to confirm a diagnosis. But for COVID-19 screening, such follow-up has been rare because testing resources are scarce or because other testing methods are prioritized for the sickest patients. Here's a look at the massive impact infection rates can have on the predictive value of these tests for individuals.
On supporting science journalism
If you're enjoying this article, consider supporting our award-winning journalism by subscribing. By purchasing a subscription you are helping to ensure the future of impactful stories about the discoveries and ideas shaping our world today.
Credit: Amanda Montañez
Read more about the coronavirus outbreak from Scientific American here. And read coverage from our international network of magazines here.
