Lab mice whose brains were injected with cells from schizophrenia patients became afraid of strangers, slept fitfully, felt intense anxiety, struggled to remember new things, and showed other signs of the mental disorder, scientists reported on Thursday.
The latest advance in “chimeras,” animals created by transplanting cells from one species into another, demonstrated the value of the technique, scientists not involved in the study said, but is likely to draw renewed attention to a controversial field that opponents see as deeply immoral and undermining the natural order.
Under a 2015 moratorium, the National Institutes of Health does not fund research that transplants human stem cells into early embryos of other animals. When the NIH asked for public comment on lifting the moratorium, it received nearly 20,000 responses, almost all objecting to “grossly unethical research”; many mentioned Frankenstein.
On supporting science journalism
If you're enjoying this article, consider supporting our award-winning journalism by subscribing. By purchasing a subscription you are helping to ensure the future of impactful stories about the discoveries and ideas shaping our world today.
But the new study, in Cell Stem Cell, injected human cells into newborn mice, not embryos. It received funding from the NIH as well as private foundations, to unravel how brain development goes off the rails to cause schizophrenia. Although the prevailing idea has been that the devastating disease, which strikes some 1 percent of U.S. adults, is primarily caused by something going wrong with neurons, the scientists suspected the brain’s support cells, called glia.
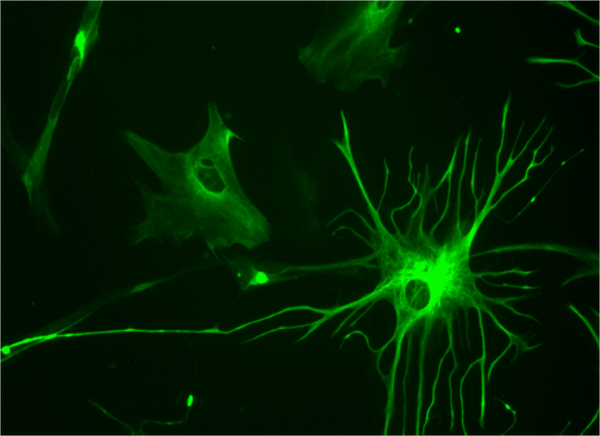
They started with skin cells from five people who had developed schizophrenia as children (it more typically strikes young adults) and three healthy volunteers. Using now-standard techniques, the researchers first turned the skin cells into stem cells very much like those in human embryos and next into human glia-making cells, then injected those into the brains of a few dozen newborn mice and watched what happened.
In short, nothing good.
Compared with glia from healthy people, glia-making cells from those with schizophrenia zipped through the mouse brains, said Dr. Steven Goldman, of the University of Rochester Medical Center, who led the research. The cells didn’t linger long enough to perform one of their chief functions: slathering a fatty molecule called myelin onto neurons like Tom Sawyer whitewashing a picket fence. Myelin enables neurons to carry the electrical signals that constitute thoughts and feelings. Schizophrenic brains have abnormally low myelination, especially when the disease strikes in childhood; defective glia may be why.
Glia-making cells from people with schizophrenia also mostly failed to turned into astrocytes, which help neurons connect and determine when those connections, or synapses, fire. When the cells did turn into astrocytes, they were misshapen. “They don’t develop normally,” Goldman said. Since astrocytes set synapses’ firing rhythms, “the synapses are now basically marching to their own beat, and you end up with a very uncoordinated network.” That can be catastrophic for a developing brain, scrambling its construction and function. “It’s easy to see how these brains don’t work right,” Goldman said.
To trace the source of the problem, the scientists analyzed what genes in the glia from people with schizophrenia were turned on and off. They found 118 genes that were on when they should have been off or off when they should have been on, compared with glia from healthy people.
The aberrantly silenced DNA included some identified in a landmark study of schizophrenia genetics, such as those that turn glia into astrocytes, are involved in myelination, or allow synapses to transmit signals. The abnormal gene expression impairs the formation of synapses so severely as to cause “structural havoc” in the brain’s wiring, Goldman and his colleagues wrote.
That affected the mice’s behavior. Compared with mice with cells from healthy people as well as non-chimera mice, those whose brains had human schizophrenia cells were more afraid to explore a maze, more anxious, more antisocial, less able to feel pleasure (from sipping sugar water), worse at remembering, and more sleepless — all of which characterize people with schizophrenia, too.
In addition to shedding light on how abnormal glia can cause schizophrenia, the study underlined how readily mouse brains accept human cells. The transplants outcompete the mice’s glia, taking their place in the developing brain until “almost all of the glia are human,” Goldman said.
That success represents a dilemma for neuroscience, said bioethicist Hank Greely of Stanford University: “When you make a chimera with human cells in its brain, the closer the resulting brain is to human” in structure and function and “the greater the ethical and public concern.” But because the mice had human glia but not human neurons, he said, “we would have fewer concerns about any conceivable ‘humanization’ of the mouse.”
Republished with permission from STAT. This article originally appeared on July 20, 2017